I have been an otolaryngologist for extra than two a long time. My people explain to me they want more purely natural seem, far more pleasure of new music, and most of all, greater comprehension of speech, especially in options with track record noise—the so-referred to as
cocktail bash issue. For 15 years, my group at the University of Göttingen, in Germany, has been collaborating with colleagues at the College of Freiburg and beyond to reinvent the cochlear implant in a strikingly counterintuitive way: making use of light.
We identify that today’s cochlear implants operate up towards challenging restrictions of engineering and human physiology. So we’re establishing a new form of cochlear implant that employs gentle emitters and genetically altered cells that reply to light. By applying specific beams of gentle as a substitute of electrical recent to encourage the cochlear nerve, we expect our optical cochlear implants to much better replicate the comprehensive spectral mother nature of appears and far better mimic organic hearing. We goal to begin clinical trials in 2026 and, if all goes well, we could get regulatory approval for our device at the starting of the following 10 years. Then, folks all above the world could get started to listen to the mild.
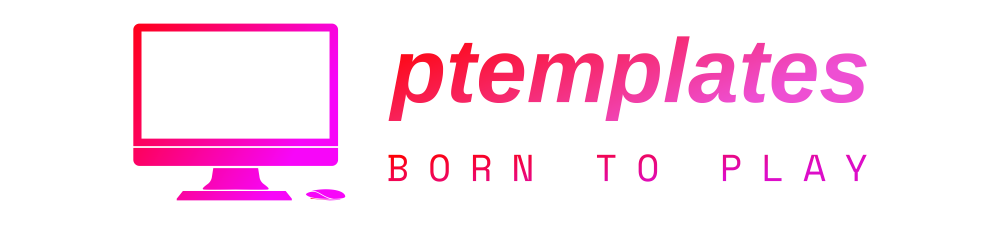
 These 3D microscopic images of mouse ear anatomy display optical implants [dotted lines] twisting by means of the intricate structure of a usual cochlea, which is made up of hair cells in deafness, these cells are lost or ruined. At remaining, the hair cells [light blue spiral] connect to the cochlear nerve cells [blue filaments and dots]. In the middle and right illustrations or photos, the bony housing of the mouse cochlea surrounds this delicate arrangement.Daniel Keppeler
These 3D microscopic images of mouse ear anatomy display optical implants [dotted lines] twisting by means of the intricate structure of a usual cochlea, which is made up of hair cells in deafness, these cells are lost or ruined. At remaining, the hair cells [light blue spiral] connect to the cochlear nerve cells [blue filaments and dots]. In the middle and right illustrations or photos, the bony housing of the mouse cochlea surrounds this delicate arrangement.Daniel Keppeler
How cochlear implants do the job
Some
466 million people around the world go through from disabling listening to reduction that demands intervention, according to the Entire world Well being Group. Listening to reduction predominantly benefits from destruction to the cochlea caused by illness, noise, or age and, so considerably, there is no overcome. Listening to can be partly restored by hearing aids, which basically offer an amplified version of the audio to the remaining sensory hair cells of the cochlea. Profoundly hearing-impaired individuals advantage additional from cochlear implants, which, as described earlier mentioned, skip in excess of dysfunctional or missing hair cells and right stimulate the cochlear, or auditory, nerve.
In the 2030s, men and women all about the planet could begin to hear the light.
Today’s cochlear implants are the most successful neuroprosthetic to date. The 1st product was authorised by the U.S. Foods and Drug Administration in the 1980s, and
almost 737,000 devices had been implanted globally by 2019. Nevertheless they make constrained use of the neurons obtainable for sound encoding in the cochlea. To recognize why, you initial need to have to recognize how pure hearing will work.
In a performing human ear, audio waves are channeled down the ear canal and established the ear drum in motion, which in flip vibrates very small bones in the middle ear. These bones transfer the vibrations to the internal ear’s cochlea, a snail-shaped framework about the dimension of a pea. Within the fluid-loaded cochlea, a membrane ripples in reaction to audio vibrations, and individuals ripples transfer bundles of sensory hair cells that venture from the area of that membrane. These movements bring about the hair cells to release neurotransmitters that cause an electrical sign in the neurons of the cochlear nerve. All these electrical signals encode the seem, and the signal travels up the nerve to the brain. No matter of which seem frequency they encode, the cochlear neurons signify seem depth by the amount and timing of their electrical alerts: The firing charge can reach a few hundred hertz, and the timing can achieve submillisecond precision.
Hair cells in distinctive parts of the cochlea answer to different frequencies of sound, with these at the base of the spiral-shaped cochlea detecting high-pitched appears of up to about 20 kilohertz, and individuals at the major of the spiral detecting very low-pitched sounds down to about 20 Hz. This frequency map of the cochlea is also out there at the amount of the neurons, which can be believed of as a spiraling array of receivers. Cochlear implants capitalize on this framework, stimulating neurons in the base of the cochlea to produce the perception of a higher pitch, and so on.
A business cochlear implant right now has a microphone, processor, and transmitter that are worn on the head, as very well as a receiver and electrodes that are implanted. It commonly has amongst 12 and 24 electrodes that are inserted into the cochlea to directly encourage the nerve at distinctive factors. But the saline fluid within just the cochlea is conductive, so the present-day from every single electrode spreads out and will cause wide activation of neurons throughout the frequency map of the cochlea. Mainly because the frequency selectivity of electrical stimulation is limited, the excellent of synthetic hearing is minimal, as well. The all-natural course of action of hearing, in which hair cells result in exact details on the cochlear nerve, can be assumed of as playing the piano with your fingers cochlear implants are more equal to participating in with your fists. Even worse, this large stimulation overlap limits the way we can promote the auditory nerve, as it forces us to activate only 1 electrode at a time.
How optogenetics will work
The strategy for a better way commenced back in 2005, when I commenced hearing about a new system remaining pioneered in neuroscience referred to as
optogenetics. German scientists were being among the the 1st to learn light-delicate proteins in algae that regulated the movement of ions throughout a cellular membrane. Then, other study groups began experimenting with taking the genes that coded for such proteins and working with a harmless viral vector to insert them into neurons. The upshot was that shining a light-weight on these genetically altered neurons could trigger them to open their voltage-gated ion channels and as a result fireplace, or activate, letting researchers to directly manage living animals’ brains and behaviors. Considering that then, optogenetics has turn into a major resource in neuroscience study, and clinicians are experimenting with health care programs like eyesight restoration and cardiac pacing.
I’ve extended been fascinated in how audio is encoded and how this coding goes completely wrong in hearing impairment. It transpired to me that stimulating the cochlear nerve with light-weight instead of electrical power could provide substantially more specific regulate, simply because mild can be tightly concentrated even in the cochlea’s saline environment.
We are proposing a new sort of implanted professional medical device that will be paired with a new kind of gene remedy.
If we used optogenetics to make cochlear nerve cells mild sensitive, we could then precisely hit these targets with beams of lower-electrical power light-weight to create substantially finer auditory sensations than with the electrical implant. We could theoretically have extra than five moments as several targets spaced in the course of the cochlea, possibly as numerous as 64 or 128. Audio stimuli could be electronically split up into numerous a lot more discrete frequency bands, supplying users a substantially richer practical experience of sound. This standard notion had been taken up earlier by
Claus-Peter Richter from Northwestern University, who proposed specifically stimulating the auditory nerve with large-energy infrared mild, however that idea wasn’t confirmed by other laboratories.
Our idea was remarkable, but my collaborators and I noticed a host of difficulties. We were being proposing a new form of implanted health care machine that would be paired with a new type of gene therapy, the two of which must meet up with the maximum basic safety expectations. We’d need to have to identify the best light-weight resource to use in the optogenetic procedure and how to transmit it to the good places in the cochlea. We experienced to uncover the appropriate gentle-delicate protein to use in the cochlear nerve cells, and we experienced to figure out how ideal to produce the genes that code for individuals proteins to the ideal areas of the cochlea.
But we have designed fantastic development more than the years. In 2015, the European Study Council gave us a vote of self-confidence when it
funded our “OptoHear” project, and in 2019, we spun off a company called OptoGenTech to function towards commercializing our system.
Channelrhodopsins, micro-LEDs, and fiber optics
Our early proof-of-concept experiments in mice explored the two the biology and know-how at participate in in our mission. Discovering the suitable mild-delicate protein, or channelrhodopsin, turned out to be a extensive course of action. Lots of early attempts in optogenetics utilised
channelrhodopsin-2 (ChR2) that opens an ion channel in reaction to blue mild. We utilized it in a proof-of-idea experiment in mice that shown that optogenetic stimulation of the auditory pathway furnished far better frequency selectivity than electrical stimulation did.
In our ongoing lookup for the greatest channelrhodopsin for our goal, we tried using a ChR2 variant identified as
calcium translocating channelrhodopsin (Capture) from the Max Planck Institute of Biophysics lab of Ernst Bamberg, 1 of the world pioneers of optogenetics. We delivered Capture to the cochlear neurons of Mongolian gerbils utilizing a harmless virus as a vector. We following experienced the gerbils to react to an auditory stimulus, teaching them to keep away from a particular space when they read a tone. Then we deafened the gerbils by making use of a drug that kills hair cells and inserted a little optical cochlear implant to promote the gentle-sensitized cochlear neurons. The deaf animals responded to this light-weight stimulation just as they had to the auditory stimulus.
The optical cochlear implant will allow individuals to select out voices in a busy conference and appreciate the subtleties of their preferred songs.
On the other hand, the use of Catch has two complications: Initially, it demands blue light-weight, which is linked with
phototoxicity. When gentle, specifically significant-energy blue mild, shines directly on cells that are ordinarily in the dark of the body’s inside, these cells can be weakened and ultimately die off. The other issue with Catch is that it’s sluggish to reset. At entire body temperature, when Capture is activated by gentle, it requires about a dozen milliseconds to near the channel and be completely ready for the subsequent activation. Such slow kinetics do not aid the exact timing of neuron activation required to encode audio, which can involve more than a hundred spikes for every next. Many folks stated the kinetics of channelrhodopsins produced our quest impossible—that even if we received spectral resolution, we’d drop temporal resolution. But we took those uncertainties as a sturdy motivation to glimpse for faster channelrhodopsins, and ones that react to crimson mild.
We have been psyched when a leader in optogenetics,
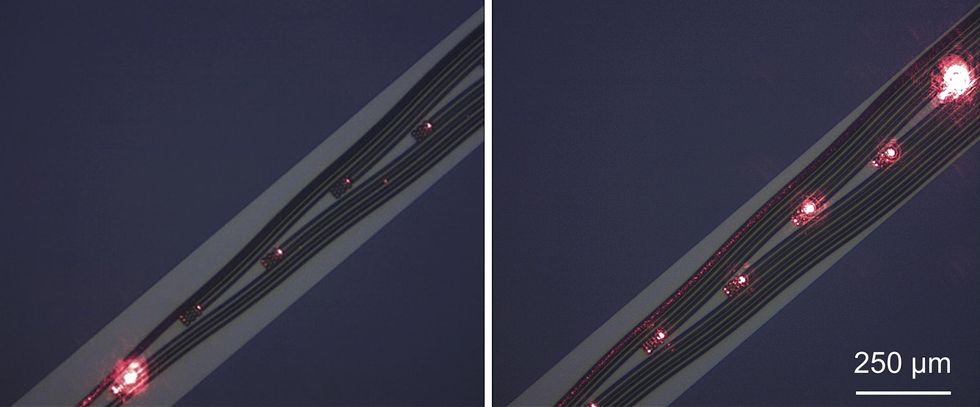
Edward Boyden at MIT, found out a quicker-acting channelrhodopsin that his group identified as Chronos. Even though it still needed blue gentle for activation, Chronos was the swiftest channelrhodopsin to day, using about 3.6 milliseconds to shut at place temperature. Even much better, we found that it closed in about 1 ms at the hotter temperature of the entire body. Nevertheless, it took some excess methods to get Chronos doing work in the cochlea: We had to use impressive viral vectors and specified genetic sequences to boost the supply of Chronos protein to the mobile membrane of the cochlear neurons. With these tips, both of those one neurons and the neural populace responded robustly and with fantastic temporal precision to optical stimulation at bigger premiums of up to about 250 Hz. So Chronos enabled us to elicit in the vicinity of-organic rates of neural firing, suggesting that we could have both frequency and time resolution. But we still needed to obtain an ultrafast channelrhodopsin that operated with more time wavelength mild.
We teamed up with Bamberg to just take on the problem. The collaboration targeted Chrimson, a channelrhodopsin 1st described by Boyden that is finest stimulated by orange mild. The
first effects of our engineering experiments with Chrimson were being quickly Chrimson (f-Chrimson) and incredibly speedy Chrimson (vf-Chrimson). We ended up pleased to find out that f-Chrimson enables cochlear neurons to reply to pink light reliably up to stimulation rates of about 200 Hz. Vf-Chrimson is even speedier but is a lot less very well expressed in the cells than f-Chrimson is so considerably, vf-Chrimson has not shown a measurable edge more than f-Chrimson when it will come to superior-frequency stimulation of cochlear neurons.
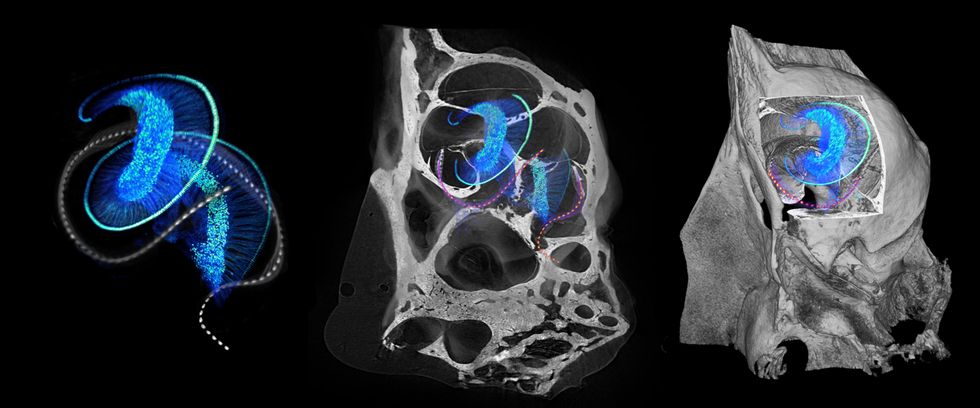
 This versatile micro-LED array, fabricated at the University of Freiburg, is wrapped all over a glass rod which is 1 millimeter in diameter. The array is revealed with its 144 diodes turned off [left] and working at 1 milliamp [right]. College of Freiburg/Frontiers
This versatile micro-LED array, fabricated at the University of Freiburg, is wrapped all over a glass rod which is 1 millimeter in diameter. The array is revealed with its 144 diodes turned off [left] and working at 1 milliamp [right]. College of Freiburg/Frontiers
We have also been exploring our solutions for the implanted gentle supply that will set off the optogenetic cells. The implant should be smaller plenty of to fit into the restricted house of the cochlea, stiff sufficient for surgical insertion, still adaptable enough to gently adhere to the cochlea’s curvature. Its housing need to be biocompatible, clear, and strong sufficient to last for many years. My collaborators
Ulrich Schwarz and Patrick Ruther, then at the University of Freiburg, started factors off by creating the initially micro-gentle-emitting diodes (micro-LEDs) for optical cochlear implants.
We located micro-LEDs helpful for the reason that they are a really mature commercial technological innovation with superior electricity performance. We done
severalexperiments with microfabricated skinny-film micro-LEDs and demonstrated that we could optogenetically stimulate the cochlear nerve in our focused frequency ranges. But micro-LEDs have negatives. For just one factor, it is difficult to set up a adaptable, transparent, and sturdy airtight seal close to the implanted micro-LEDs. Also, micro-LEDs with the optimum efficiency emit blue mild, which delivers us back to the phototoxicity problem. That is why we’re also wanting at another way ahead.
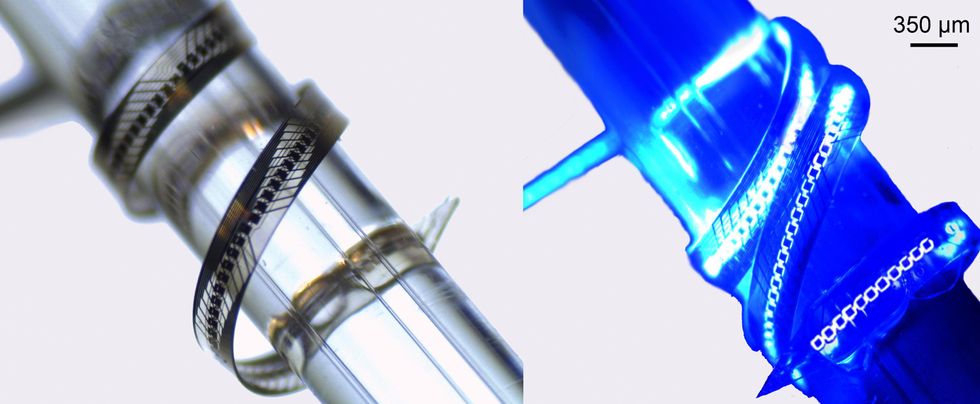
Instead of obtaining the semiconductor emitter by itself into the cochlea, the choice strategy puts the light source, this sort of as a laser diode, farther away in a hermetically sealed titanium housing. Optical fibers then deliver the mild into the cochlea and to the mild-delicate neurons. The optical fibers ought to be biocompatible, long lasting, and adaptable ample to wind by way of the cochlea, which may perhaps be complicated with normal glass fibers. There’s attention-grabbing ongoing research in adaptable polymer fibers, which might have far better mechanical features, but so considerably, they haven’t matched glass in effectiveness of light-weight propagation. The fiber-optic method could have performance drawbacks, due to the fact we’d reduce some mild when it goes from the laser diode to the fiber, when it travels down the fiber, and when it goes from the fiber to the cochlea. But the solution seems promising, as it makes sure that the optoelectronic parts could be safely sealed up and would very likely make for an straightforward insertion of the flexible waveguide array.
 Another design possibility for optical cochlear implants is to use laser diodes as a gentle resource and pair them with optical fibers created of a versatile polymer. The laser diode could be safely encapsulated outside the house the cochlea, which would decrease issues about heat, when polymer waveguide arrays [left and right images] would curl into the cochlea to provide the gentle to the cells.OptoGenTech
Another design possibility for optical cochlear implants is to use laser diodes as a gentle resource and pair them with optical fibers created of a versatile polymer. The laser diode could be safely encapsulated outside the house the cochlea, which would decrease issues about heat, when polymer waveguide arrays [left and right images] would curl into the cochlea to provide the gentle to the cells.OptoGenTech
The street to medical trials
As we look at assembling these elements into a industrial clinical gadget, we first look for sections of existing cochlear implants that we can undertake. The audio processors that perform with today’s cochlear implants can be tailored to our goal we’ll just require to break up up the signal into far more channels with more compact frequency ranges. The exterior transmitter and implanted receiver also could be very similar to current systems, which will make our regulatory pathway that a lot less difficult. But the definitely novel sections of our system—the optical stimulator and the gene treatment to supply the channelrhodopsins to the cochlea—will require a great sum of scrutiny.
Cochlear implant surgical procedure is pretty experienced and typically can take only a pair of several hours at most. To preserve points straightforward, we want to keep our procedure as close as doable to present surgeries. But the critical part of the operation will be quite distinct: Instead of inserting electrodes into the cochlea, surgeons will 1st administer viral vectors to deliver the genes for the channelrhodopsin to the cochlear nerve cells, and then implant the gentle emitter into the cochlea.
Due to the fact optogenetic therapies are just starting to be analyzed in scientific trials, there’s nonetheless some uncertainty about how most effective to make the system perform in humans. We’re even now wondering about how to get the viral vector to provide the required genes to the appropriate neurons in the cochlea. The viral vector we’ve utilised in experiments consequently far, an
adeno-linked virus, is a harmless virus that has previously been accepted for use in many gene therapies, and we’re employing some genetic methods and area administration to concentrate on cochlear neurons particularly. We have currently begun gathering knowledge about the stability of the optogenetically altered cells and regardless of whether they’ll will need repeated injections of the channelrhodopsin genes to remain responsive to light-weight.
Our roadmap to medical trials is really bold. We’re functioning now to finalize and freeze the design of the system, and we have ongoing preclinical research in animals to check out for phototoxicity and verify the efficacy of the basic plan. We goal to commence our initially-in-human research in 2026, in which we’ll obtain the safest dose for the gene therapy. We hope to start a substantial stage 3 clinical demo in 2028 to collect details that we’ll use in distributing the gadget for regulatory acceptance, which we could earn in the early 2030s.
We foresee a upcoming in which beams of gentle can provide prosperous soundscapes to men and women with profound listening to reduction or deafness. We hope that the optical cochlear implant will allow them to decide out voices in a hectic assembly, recognize the subtleties of their favorite tracks, and take in the entire spectrum of sound—from trilling birdsongs to booming bass notes. We believe this engineering has the possible to illuminate their auditory worlds.
From Your Site Content articles
Related Posts Close to the Web